Our Investigation
BBC Story October 2022 - No one joined the dots - https://www.bbc.co.uk/news/uk-63298087
Within an hour or two of Harry's birth, two consultants, one Paediatric and one Obstetric told us there would be an investigation called a Root Cause Analysis (RCA) to find out what had happened. The day after Harry died, November 10th 2017, Sarah and Tom asked the consultant in charge of Harry's care at William Harvey Hospital, Dr Kwok Sean Mun, whether Harry's death would be reported to the coroner. They were told no, there was no requirement as the cause of death was known, HIE Grade 3 (Severe Brain damage). Subsequently, the Trust were asked on numerous occasions, but they refused including in writing in a letter, again in the RCA and in a recorded meeting.
We were deeply uneasy as the RCA was being conducted by Consultant, Dr Clare Redfearn who was the clinical lead of the maternity ward and was effectively investigating her own staff, colleagues and indeed, policies and procedures she may well have instigated. It later transpired that Dr Redfearn had only become a consultant 2 months before Harry's death and this was her first and only RCA. We raised our concerns about transparency with the Trust but they were dismissed.
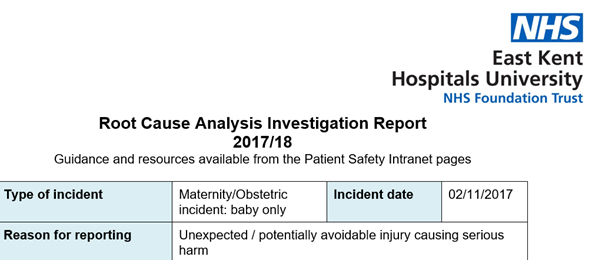
The Trust told us that the RCA was overseen by the head of Women's Health, Dr John Seaton and that he assisted Clare Redfearn with the RCA. We were still uneasy as, in effect, he was the overall man in charge of the unit and Clare Redfearn's boss. The RCA also included Matron Peyma Hajilou, who was actually on duty the morning Harry was born. Looking at the RCA we were sent (Front Page Here) you can see the lead investigators were Dr Clare Redfearn and Dr Sean Mun, assisted by Dr Abigail Price, Peyma Hajilou and Edel Ewart. Of these, Clare Redfearn is clinical lead of Maternity, Sean Mun was treating Harry as was Abigail Price and Peyma Hajilou was on duty in the ward where Harry was born on that morning. You can see why we were uneasy. Later, when we raised this issue, Dr Abigail Price asked for her name to be removed from the RCA as she said she wasn't part of the investigation team?
We reported the whole of Harry's story as we knew it to the Care Quality Commission (CQC) and although we had acknowledgement emails there was nothing more at this stage and they didn't seem very interested at all. We also advised our MP Sir Roger Gale who was really helpful and supportive but wanted to let due process happen first, which was of course fair.
The RCA seemed to take forever. We had sporadic updates but no one would tell us what was going on. The investigation's 60 day deadline was breached and then extended to 90 days as the case was said to be "very complex" On March 6th 2018 we were finally sent the RCA in hard copy only (so we had to scan and photocopy) and an invitation to go and talk about the report at 2.00 pm on March 14th, we duly accepted and spent the time in between, day and night, pouring over the 67 page report. At first sight it seemed thorough enough, but when read in detail, it threw up numerous troubling questions.
We arrived at the Trust in good time on 14th and at 2.00 pm were taken to a meeting room. It wasn't ready and we helped them to arrange chairs and tables for everyone to sit on and to arrange water for the table. There were 5 of us and there was due to be 6 members of the Trust team including 4 consultants, Dr Clare Redfearn, Dr Anastasia Goumenou, Dr Abigail Price and Dr Kwok Sean Mun, a corporate governance officer Annie Oakley, who was the meeting Chair and a midwife coordinator Karen Keatley; this was a very big meeting. One of the consultants turned up 10 minutes late and Dr Mun the neonatologist and joint lead investigator was still at William Harvey Hospital 40 miles away and eventually arrived an hour late. We had to start without him...........
The meeting was recorded at our request. The meeting was so poorly chaired, consultants were arguing with each other and at one point, the consultant in charge of the RCA had to leave the room to compose herself as she was sobbing. We asked a good number of searching questions regarding who signed off the locum doctor but they had no answers, all they could say was his CV was signed off by a consultant. Around a month later we discovered that he hadn't been signed off by anyone at all, in fact, he had not been assessed by the Trust in any way. We asked again about calling the coroner and were told very definitely by Dr Kwok Sean Mun and Dr Abigail Price, in fact for a full 12 minutes, that referral to the coroner was not required, it was stated by Dr Sean Mun, consultant neonatologist said - (and we quote verbatim) -
"We know that there was an event that caused Harry to have eventual lack of oxygen to the brain. He was delivered in a poor condition, there were problems getting resuscitation going because of significant mucus and again one event after another, this is very very clear process that there’s lack of oxygen, this has led to brain damage. So if you ask any neonatologist in the country they will say the same thing that there was a clear sentinel event followed by a clear course leading to a clear endpoint and I believe if you consult the Gov website I think you have a clear cause. It’s not the events leading up to the cause, if you have a clear cause of death." "I think if we have a clear cause of death by and large we do not involve the Coroner."
We pushed hard and and they eventually agreed to inform the coroner On March 14th 2018. We asked a lot more questions that day, and we left the meeting after three and a half hours with far more questions than when we arrived. It was from this point that we all knew what we had suspected for a long time, Harry's birth and what had surrounded it had been covered up and we were determined to discover the truth.
The morning after our March 14th meeting, we were so disillusioned by what we had seen and heard that we reported Harry's death to the coroner ourselves (HERE), we added a note to say that the Trust had also promised to report it, but that we had little faith they would actually do so and that we thought their investigation was a cover up. We were right, we had to chase the Medical Director twice. He eventually said if it hadn't been done, he would do it himself.
It wasn't until April 20th 2018 that Dr Sean Kwok Mun from the Trust finally reported Harry's death to the coroner. This was well over 5 weeks after they had promised to do so and 23 weeks after Harry had died.
We had heard about the Healthcare Safety Investigation Branch (HSIB) and we sent the details of Harry's case to them. Harry was born too early for their new maternity investigations, these started in April 2018, so we had to make a very good case indeed. Following a raft of emails, telephone calls and us giving enough evidence to them, to persuade them that there was national learning to come from Harry's case, they agreed to take Harry's case on as a national investigation. They started their investigation in late May 2018.
Following on from our March 14th meeting and the subsequent questions grid created by the Trust, they agreed to have Harry and Sarah's notes looked at by Dartford and Gravesham Trust so that "independent" eyes could at last be cast across them. This had already been done by Maidstone and Tunbridge Wells Trust but in their report they complained of not being sent any hospital patient records or scans, only the actual RCA report written by the Trust.
The report from Dr Mark Waterstone at Dartford and Gravesham came back and was critical of many aspects of the care given including the interpretation of CTG scans, he also indicated that had Harry been resuscitated effectively he may have survived intact. What surprised us and we believe the Trust too, was the final comment "There appears to have been inadequate neonatal resuscitation which requires the expertise of a Neonatologist to review with authority." We sent this report to the coroner to add to the evidence we had already provided into Sarah and Harry's care. We immediately asked the Trust to get the neonatology report done too and, to be fair, they had realised that we would need this and had already set this in motion, again via Dartford and Gravesham Trust.
At 13.36 on Saturday 21st of July 2018 we received an email from the Medical Director Dr Paul Stevens.
"The independent neonatologist has completed his review and I promised to share this with you. I'm really sorry because this will be extremely upsetting for you as a family to read and again I apologise for what we as an organisation have subjected your family to over the last several months." The enclosed report from Dr Bokhari was a devastating read. It described a largely chaotic resuscitation where records and timings were not kept and the expert said "I would recommend a significant review of the abilities of the staff in hospital to establish and maintain an airway of a new born baby including midwives, Neonatal nurses and all junior doctors." This was devastating
news, despite all of what Harry had been through, he could and should have survived if the resuscitation had been carried out competently. This report was also sent to the coroner.
At the end of August an Inquest was agreed by the Chief Coroner for England, Mark Lucraft QC, and we were invited to a Pre-Inquest Review (PIR) on November 6th 2018. The coroner went through witnesses required and Interested Persons (IP's) and asked for submissions regarding Article 2 of the European Convention on Human Rights - Right to life. We argued for Article 2 as it would have significant implications for the conclusions of the inquest and the recommendations the Coroner could make about the failings of the Trust. The Trust argued strongly against it, Article 2 was not something they wanted at all. The coroner was persuaded by the Trusts arguments and not ours, so Article 2 was ruled out but the coroner said he would keep an open mind if any evidence changed. Harry's inquest was due to be held at the end of February/beginning of March 2019. Both the paediatric and Obstetric Registrar's were made into IP's (Interested Persons) by the coroner’s court.
We also reported these doctors to the GMC for investigation into malpractice. They started with the Locum Obstetric Registrar Dr Christos Spyroulis who had carried out Sarah's Caesarean section. After many months they found him guilty of malpractice and put 13 undertakings against his name. The summary of the decision in full is here
We decided there was evidence of deficiencies in the following areas of clinical performance; recognising and working within the limits of his competence; relationships with patients; record keeping; assessment and clinical management of patients; and operative/technical skills. In reaching this conclusion we took into account concerns raised in a complaint, information provided by Dr Spyroulis’ NHS body and the opinion of an appropriate expert.
The paediatric Registrar as well as the Obstetric consultant were also being investigated by the GMC for malpractice. Later, the Paediatric Registrar left the country to go back to Sri-Lanka and revoked his licence to practice and was not pursued. The GMC found that the Consultant's fitness to practice was impaired at the time. However, she had reflected and had a blemish free past, so no action at all was taken.
"It is now over three years since the sad events. There have been no previous or subsequent concerns identified regarding Dr Goumenous’ fitness to practice and there is good evidence of her insight, remediation and remorse. The GMC expert (and others who have reviewed the case), have clearly pointed out the expectations of an on-call obstetric consultant, and that Dr Goumenou’s failure to attend when told about the delay in delivery and need for intervention in theatre was seriously below the expected standard, and we agree that Dr Goumenou’s fitness to practise may have been impaired at the time. However, given the above remediation, we are of the view that there is no realistic prospect of demonstrating that she poses an on-going risk to patient safety and is not currently fit to practise."
It seems that, although the GMC agreed that her fitness to practice was impaired at the time and that her actions were seriously below the expected standard, there was no need for any warning or sanction. Quite extraordinary.
In the background HSIB were still carrying out their investigation; we were also looking at just about anything we could get our hands on. We found that on the Trust's website there were a complete set of board meeting actions and Integrated Performance Reports (IPR) which we downloaded and examined in detail, mainly through searching for "maternity" or similar key words.
After an awful lot of work trawling through reports and the internet, it became apparent that back in June 2016 the Trust had raised a Corporate Risk Register entry CRR26 that described "Regulatory non compliance in Obstetrics and Maternity" It described the cause as "Reports from both the Royal College of Obstetrics and Gynaecologists (RCOG) and the Local Supervisory Authority (LSA) identified gaps in regulatory compliance and also other areas of improvement in maternity services." it went on to describe the Inherent Risk Score as "Extreme". The risk was due to be mitigated by 31st October 2016.
We spent time and energy looking at as many Trust board reports and IPR's as we could get, we downloaded them all and poured over them. It emerged that the Trust had not mitigated the risk by October 31st as intended at all. In fact by February 2017 they reported that there were difficulties, so they brought in another entry called CRR48. We were spellbound by what we were discovering. CRR48 had a new start date but the same wording, by April 2017 a report noted that CRR48 had subsumed CRR26 as they were basically the same thing. Various dates for completion came and went but at no point all the way up to April 2019 was the risk reported as mitigated and complete.
We notified the coroner and the CQC of our new findings.
In August of 2018, the CQC local inspector wrote back to say that she had taken advice from senior management and that there was nothing for the CQC to look at as it all centred around one individual's error. SEE HERE We wrote back thanking her for her consideration but pointed out clear systemic issues and hoped she didn't mind, but I had copied in the head of hospital inspections Professor Ted Baker as we felt further senior opinion was required. A week or two later we got a response from Professor Baker thanking us for the information and saying that their Inspection Manager for the South East would be in touch to arrange a meeting.
We looked at everything we could find online using Google to look for the nuggets of information we knew would be out there somewhere. It seemed that the Trust had issues in maternity as far back as at least the end of 2013.
In 2014 the CQC wrote -
The Chief Executive told us the maternity strategy consultation had been completed and the reconfiguration implemented successfully. However, we found that there was a disconnect between the strategy and the organisation in general and the maternity services at an operational level.
There was no mechanism to ensure that all clinical incidents were reported as there was no systematic checking that a form had been submitted for every clinical incident. This identifies a potential for under-reporting harms and near misses within the service as reporting an incident allows the trust to understand the risks and improve safety for patients.
Staff spoken with were not aware of any complaints across the units so not involved in learning the lessons from these.
We found that the risk register for maternity was across all sites and the most recent version we saw had an entry for a moderate 'risk of harm to women as a result of inadequate midwife-patient ratio'. This was a risk that had been created by decisions taken at a divisional level not being fully informed by the experience at ward level and perhaps not reviewed in a timely way.
Local CCG reports told us that the number and themes of serious incidents had prompted talks with the Trust and NHS England (NHSE). This led to a risk summit and then the RCOG were commissioned to carry out a full audit which prompted the risk entry mentioned earlier.
The risk register entry prompted us to ask for a copy of the RCOG report that had led to the risk entry CRR26 and so we raised a Freedom of Information request to get a copy. After around 4 weeks the response came through from their FOI office with a link to the report which we downloaded. We were staggered by what we read. The report had been researched by 5 RCOG assessors in November 2015, 2 full years before Harry was born.
This was the introduction to the RCOG Audit report published in February 2016, researched in November 2015. It clearly shows that there were already serious concerns known even BEFORE the commissioning of the audit.
INTRODUCTION
This review has been commissioned by Dr Paul Stevens, Consultant Nephrologist and Medical Director of East Kent Hospital’s University NHS Foundation Trust, following concerns about the working culture within women’s health services including relationships and communication between midwives and obstetricians. Issues of concern are an inconsistent compliance with national standards amongst obstetricians, poor governance in relation to serious incidents, staffing, education and supervision of obstetric middle grades and trainees and consultant accessibility and responsiveness. Concerns relating to consultant presence on the delivery suite as per RCOG recommendations have also been raised.
You can download the full RCOG report HERE
The report gave various examples of serious issues that they found; Poor culture, Lack of Escalation, CTG misinterpretation, induction and for us, crucially, consultants were found not to be attending ward rounds or attending over night and, they said, this was being tolerated by senior management. Towards the end of the report it said that the assessors were leaving after being assured that consultant attendance on ward would be monitored. The report told us that when consultants were found to be failing, it was not included in RCA investigations. It concerned us greatly that consultants behaviour was being hidden. When talking about trainees and the lack of engagement from consultants, it said “The assessors are concerned that this practice will result in consultants not committed to teaching and supervision to be on-call with a locum middle grade doctor, potentially of unknown competence, which could impact on the safety of care in the maternity unit” This was precisely what had happened in Harry's case, it was an exact prediction of what Sarah, Tom and Harry had been the victim of.
It seems that the RCOG were really concerned about consultants not doing as they should and not following Royal College guidelines, furthermore, they had discovered that senior management had done nothing about it; they pull no punches in their report regarding this -
(Page 39) "Failure to comply with the guidelines "consultant duty of care" should prompt the Medical Director to instigate a formal investigation into conduct allegations in line with the Trust’s procedure for dealing with conduct, capability and health issues for medical and dental staff. To-date poor consultant behaviour regarding lack of accessibility and presence on the delivery suite has not been challenged by management. Plans are that consultant presence will be monitored on both sites. "
This showed us that staff were making official complaints about consultants but senior directors were doing nothing to solve the issues. We felt that by November 2017, nearly 2 years later, they had still failed to deal with poor performing consultants.
Interestingly, on pages 6 and 7 the RCOG listed the vast number of people they interviewed. On page 7, at the end of the list, it names the only consultant who was unable to be interviewed and seemingly did not respond on email either; it was Ms Anastasia Goumenou, the consultant who, in Harry's case, failed to turn up for ward rounds and who failed to attend overnight when she should. Was this a coincidence we wondered?
The result of the RCOG report was a Corporate Risk Register entry at the Trust to say that there was an "Extreme Risk" to pregnant women and Neonates in our care" this was in place from June 2016 and due to be mitigated by October 2016 but it wasn't - the last time it could be seen in a board report the end date had been extended to March 31st 2020. But it was removed from the Board reports without any mitigation being reported.
We discussed what we had found within the family and concluded that there was very strong evidence that Trust had known all about the serious issues in maternity at the Trust for a very long time and, had they addressed them, Harry would have had a normal birth and been alive and well. This hurt us to the core.
We finally had a meeting arranged for the end of January 2019 with the CQC in London. We presented a document that highlighted all of the issues we knew and also presented the RCOG report from 2015 which they were seemingly unaware of, we left a copy with them.
Here is what we presented. They promised to investigate at the highest level and to take the maximum action they could thereafter. It wasn't until late August 2019 that we heard that Harry's case had been in front of an internal panel and had been approved for 2nd stage investigation. At this stage it looked quite likely that they were investigating a criminal case under Regulation 12 of the Health and Social Care Act 2008. Confirmation didn't come until October 1st when they wrote to the Trust and us to say they were formally investigating a Criminal charge under Regulation 12 of the Health and Social Care Act. On October 8th 2020, nearly 3 years after Harry's birth, the Trust were charged with the criminal offence of unsafe care and treatment for Harry and a second charge of unsafe care and treatment of Sarah - the case went to court in April 2021 and they were fined £1.1 million discounted to £766k following a guilty plea.
Soon after our meeting with the CQC, the HSIB report was published. Although HSIB are a "no blame" organisation who investigate in order to learn, they found 18 serious issues surrounding Harry's death. Details of the HSIB investigation are here
We learnt about a report that has to be filled out for government called MBRRACE-UK, which logs all baby and maternal deaths and babies who sustain brain damage. These reports aim to try and learn why the UK is so poor with baby deaths. We requested Harry's report on a Freedom of Information request but were told that it was not an FOI matter, as it will be in the clinical records of the patient. Our request was directed to the clinical records department but we were told the report was not there, we asked several times....... Eventually we got the report direct from MBRRACE-UK in Oxford under a FOI request to them.
When we got the report, we found it was full of wild inaccuracies. Such things as was the placenta kept was answered yes and then went on to say it was used for histology to determine the cause of death. The placenta was not kept at all as confirmed in Harry's post-mortem. The MBRRACE report said that the coroner had been called, he hadn't, rotational forceps were used, they weren't. They said that the Apgar score at 1 minute and 5 minutes was not available, they were in Harry's notes. The final part, were there any delivery complications was answered with None. We wrote to the Medical Director to ask where the information comes from for the MBRRACE report and we were told "the patients notes" but Harry and Sarah's notes showed this to be wholly untrue.
By the end of June 2019 we had a full and frank admission from the Trust's solicitors. “We have also carried out our own investigations, as a result of which the Trust accepts that the standard of care for your client, Mrs Richford and Harry, did not meet a reasonable standard, both during delivery and immediately afterwards.” The admission was so stark and unequivocal that we felt vindicated in all our investigating, whilst being disappointed that the wording "suggested" that only after their solicitors own investigation did the Trust accept what it had done was wrong. This was exacerbated a week later when we got an apology from the CEO apologising that their care had "contributed" to Harry's death. It went on to say that there was an HSIB investigation being carried out and they would comply with its findings. The HSIB report had been published to them in February, 4 months earlier yet the CEO seemed to have no clue whatsoever. The CEO later admitted to the BBC in an interview that she hadn't even seen the RCOG report until December 2019, just a month before Harry's inquest and nearly 4 years after it was published.
Acott Interview. However, she had actually mentioned it to us in a letter a year earlier??
On the first day of Harry's inquest an apology was issued to the media, not to us. This apology was a far stronger apology than anything we had received from the Trust to that point. Still they did not apologise for Sarah's care, only Harry. The coroner was highly critical that neither he or the family were sent this apology, only the media. This was an apology for the media and not for the family, seemingly to try and limit reputational damage.
The downside of an admission from the Trust is that our Conditional Fee Arrangement (CFA or "no win no fee") deal with our solicitor in Whitstable meant he could no longer come to the inquest or any PIR's as the Trust wouldn't have to pay him. He wrote to the Trust to ask if they would pay for reasonable cover for the family as the Trust would be using public funds to represent themselves, but they refused. We wrote to AvMA who are a really helpful charity but Harry's case was likely, at that stage to be a 10 day inquest and they couldn't get that much help from one barrister. Our MP, Sir Roger Gale came straight to the rescue and endorsed an application to "Advocate" the Bar Council Pro Bono unit.
Link to Advocate
Within a couple of weeks we had cover from a top barristers chambers in London.
Brick Court Chambers who were supported by solicitors Arnold and PorterLLP, one of the biggest law firms in the world. We were very fortunate indeed and will forever be indebted to Jenny, Emma, Jackie, Louise ,Giles and Daisy for their care, professionalism and the genuine love they showed our family.
We kept sending evidence to the coroner and the CQC in order to keep them abreast of matters and to try and push the coroner into finding us a date for Harry's inquest. At one point we were told that the inquest was now likely to be September/October only to be told soon after that early 2020 was now more likely. The anguish that this all caused cannot be underestimated. At last, at the beginning of August we got a date for a 2nd PIR, this was to be a full day event on October 16th 2019, at least we had some progress.
Two weeks after being told the new PIR was on October 16th we were told that our coroner had double booked with another inquest and could not now conduct Harry's inquest. We emailed our MP again, he had been really helpful with sending emails and supporting us in every regard, he had recognised that Harry's case was one of importance not only to us but the wider community. He wrote to the Chief Coroner to gently ask if anything could be done to expedite Harry's case, inevitably the response came back to say that he couldn't deal with any individual cases.
By early September we were called to an urgent PIR with a new coroner, ours had retired as he was 70 and we got a very experienced barrister coroner who certainly seemed to know his stuff, he was Christopher Sutton-Mattocks. He was a semi-retired barrister and had a great deal of experience in Article 2. At the urgent PIR he asked for submissions on Article 2 again, IP's and witnesses.
A full day PIR was then called for October 14th in Sandwich Kent and Harry's inquest was set for January 6th for 2 weeks and 2 days. Various papers were requested including policies and procedures in force when Harry died and a full statement from the Medical Director. In what can only be described as deep disrespect for the family, the Trust failed to supply this paperwork before the inquest. However, on day 2 of the inquest thy dropped over 1,000 digital pages of evidence onto our legal team. The Medical Directors statement, one of the most important statements was supplied on New Year's Eve 2019 just 2 working days before the inquest.
It wasn't until December 13th that we were sent the Coroner's expert report on midwifery. It was another devastating read. It showed that CTG's had been misinterpreted by different midwives and that Syntocinon had been overdosed. All in all, the report showed that, in the words of the expert, care fell below or well below the expected standard. The NMC investigated 7 midwives and as at September 2021 are still investigating 3.
We therefore had three coroner’s experts telling us and the court that the midwives, obstetricians and paediatricians all offered Sarah and Harry substandard care. We were left wondering how all this could happen in one place at one time unless gross systemic failings in management were to blame?
The fact that at the exact time of Harry's birth the Trust had a corporate risk entry showing known failings was not lost on us. In addition, it was at this exact time the Trust claimed they were 10 out of 10 for maternity safety and claimed well over £1 million from the NHS as a rebate. We raised this with NHS Resolutions the scheme administrators and also Sir Roger Gale MP, as we could prove it was a false claim. The Trust claimed the same 10/10 the year after.
After the Trusts year-2 claim of 10/10, NHSR audited the results in December 2019 and found that the Trust were only in fact achieving 6/10 and in the bottom 6% of Trusts. The Trust were told to repay the awarded funds. As a result, NHSR audited the year 1 claim that we had initially complained about; they found that the Trust were also in fact at 6/10 and not the 10/10 as claimed. NHSR required the Trust to repay the funds paid. Over two years this was around £2.5 million pounds.
Sir Roger Gale MP challenged Susan Acott the Trust CEO on May 9th 2019 and in her response to him on June 7th 2019 she wrote -
".....the evidence we have met the requirements was presented to our full Trust Board on two occasions and also our Quality and Safety Committee. Helpfully our new Chairman is a Professor of Obstetrics and Gynaecology, so we have absolute expertise on our Board. The evidence was peer reviewed with a Trust in West Kent, although this was not a requirement, as well as our commissioners. I have written to NHSR confirming the level of evidence and scrutiny that accompanied the Board sign-off."
She went on to write -
"We all fully appreciate and sympathise with Derek Richford. Trying to undermine the reputation of the entire hospital and deny it resources doesn't help or improve the situation for future parents and our existing staff however."
6 Months later the Trust were having to repay circa £2.1 million to the NHS following two years of false claims. But where is the accountability for such actions?
Isle of Thanet News Story on the false claim of funds
It was only after all of this that we learnt far more about the Shrewsbury and Telford investigation and Donna Ockenden. Sadly, it seemed that yet another scandal was opening up there.
We feel that the Trust has been poorly managed and governed for a good number of years. This is not good for patients or staff. Improvement will only happen when clear responsive managers have their teams working with them towards the same goals. Maternity - EKHUFT Maternity - EKHUFT Maternity - EKHUFT Maternity - EKHUFT Maternity - EKHUFT Maternity
EKHUFT Maternity - EKHUFT Maternity EKHUFT Maternity - EKHUFT Maternity - EKHUFT Maternity - EKHUFT
